Types of Heart Stents and Their Uses
A stent is a small mesh tube that is used to keep weak or narrowed arteries open. Patients suffering from coronary heart disease have narrowed and partially blocked arteries as a result of plaque buildup within the arteries. This narrowing or blockage of the arteries results in a reduced blood flow to the heart which causes the symptoms such as chest pain or angina and may even result in heart attacks.
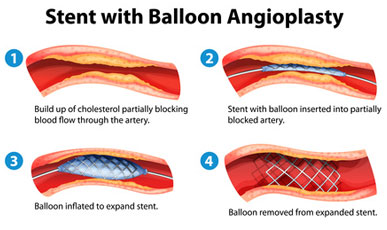
A stent is used during a surgical procedure known as angioplasty. This procedure helps to restore the flow of blood through the narrowed or blocked artery. A stent helps to support the inner wall of the artery in the years to come. These types of stents are also known as cardiac stents or coronary stents.
Stenting is a minimally invasive procedure as it does not require a large incision (as in the case of conventional coronary artery bypass surgery). Stenting is usually performed using local anesthesia and it takes approximately an hour to complete the procedure. It may however, take longer in case several stents are required. Since stenting is a minimally invasive procedure it requires much shorter recovery time when compares to coronary bypass surgery. However, it is not without its risks. You can gain a better understanding of the risks involved by looking at the evolution of stents and the many different types of stents that are available today.
Doctors started using balloon angioplasty in the late 1970s. This procedure involved inserting a balloon-tipped catheter into the artery which is then threaded to the narrowed portion of the artery. The balloon is inflated which compresses the blockage, thereby restoring the flow of blood. However, in many cases the artery would return to its previous state after the removal of the balloon. In addition to this, about 30% to 40% of all cases were affected by restenosis. Restenosis occurs when scar tissue forms on the inner wall of the artery at the site of the angioplasty. This scar tissue results in a re-narrowing of the artery over a period of time and is known as restenosis.
Stents were invented to counter the problem of restenosis. The initial wire mesh stents surrounded the balloon portion of the catheter. Once at the site of the blockage, the balloon was inflated with the mesh in place. The mesh would then lock into place and form a permanent support which would prevent the wall of the artery from collapsing. With stents, the number of cases of restenosis dropped to about 20%. Restenosis was not the only risk a patient faced. There was the possibility of blood clots forming in the stent which could result in a complete blockage of the artery. Blood thinning drugs such as aspirin were usually prescribed to counter that possibility.
To decrease the incidence of restenosis, pharmaceutical companies began coating stents with drugs that could prevent restenosis from occurring. These stents are known as "drug-eluting stents" and they were able to reduce the rate to restenosis to 10%. Drug-eluting stents were also found to be effective in treating diabetics who are at a higher risk of restenosis. Stents made out of fabric instead of metal, known as stent grafts were also developed. These are found to be more effective when used in larger arteries. However, concerns such as late in-stent thrombosis have caused a decline in the use of drug-eluting stents. FDA guidelines however, suggest that drug-eluting stents when used as directed are not associated with an increased risk of heart attack or death.
Several newer stents such as those that are gradually absorbed by the body are also under development. To decide which type of stent would be best for you, you should have a lengthy and thorough discussion with your doctor. This will help you to make an informed decision.
Reference